April 17, 2024
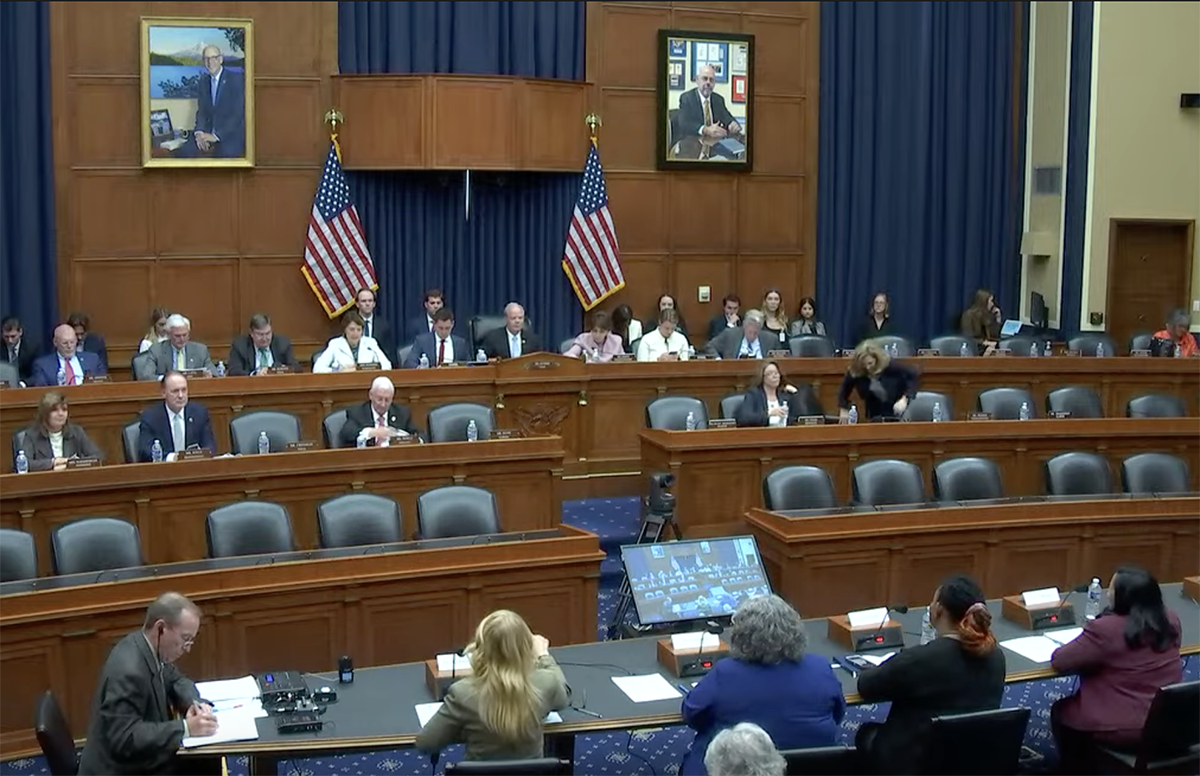
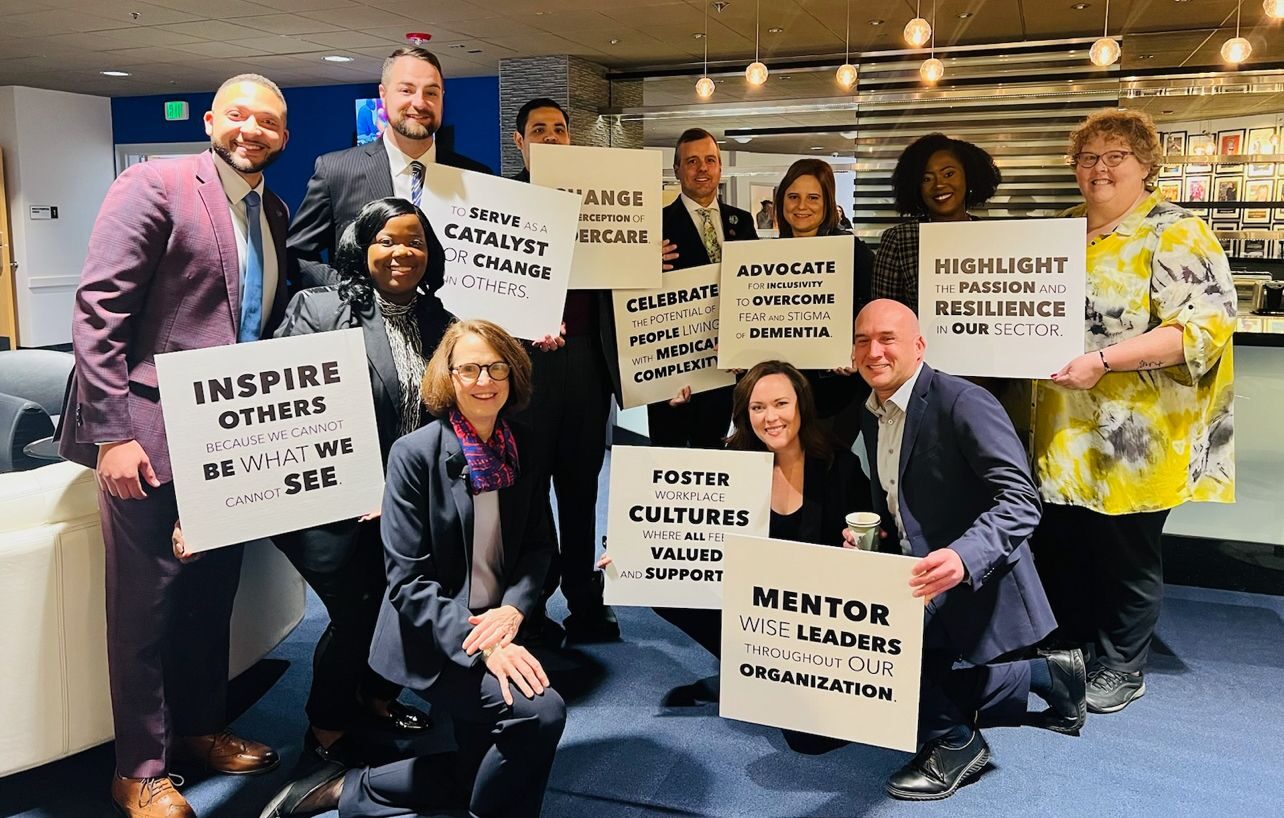
National Advocacy: LeadingAge Members ‘Speak Up and Speak Out’ on Lobby Day 2024
More than 240 members met with lawmakers and staff about critical issues including staffing mandates, housing and hospice expansion, Medicare Advantage, and more.
LEARN MORE